
Plantar fasciitis induces heel discomfort characterized as a “stabbing” sensation, particularly heightened during initial steps in the morning or while running. It can be caused by running due to repetitive stress and strain on the plantar fascia, a thick band of tissue that supports the arch of the foot.
• Overuse and Repetitive Stress: Long-distance running or engaging in activities that involve repetitive impact, such as running on hard surfaces, can subject the plantar fascia to excessive stress. Over time, this repetitive stress may lead to microtears in the fascia, causing inflammation and pain.
• Poor Foot Mechanics: Improper running form or biomechanical issues, such as overpronation (excessive inward rolling of the foot) or supination (insufficient inward rolling of the foot), can contribute to increased strain on the plantar fascia. Running with improper footwear or worn-out shoes that lack proper arch support can exacerbate these issues.
• Sudden Increases in Intensity or Duration: Rapidly increasing the intensity, duration, or frequency of running without allowing sufficient time for the feet to adapt can contribute to the development of plantar fasciitis. This is particularly common in runners who push themselves too hard or abruptly change their training regimen.
• Tight Calf Muscles and Achilles Tendon: Tightness in the calf muscles and Achilles tendon can affect the mechanics of the foot and increase stress on the plantar fascia. Runners with inflexible calf muscles may be more prone to developing plantar fasciitis.
• Inadequate Warm-Up and Stretching: Failing to properly warm up before a run or neglecting to stretch the calf muscles and plantar fascia can contribute to the development of plantar fasciitis. Adequate stretching helps improve flexibility and reduce the risk of overuse injuries.
To prevent plantar fasciitis while running, it’s essential to:
• Gradually increase running intensity and duration.
• Wear proper running shoes with adequate arch support.
• Maintain good running form and biomechanics.
• Incorporate regular stretching exercises, especially for the calf muscles and plantar fascia.
• Listen to your body and address any signs of discomfort promptly.
If symptoms of plantar fasciitis persist or worsen, it’s advisable to consult with a healthcare professional for a thorough assessment and appropriate treatment recommendations, which may include rest, ice, stretching exercises, orthotic inserts and CellStim Microcurrent Therapy
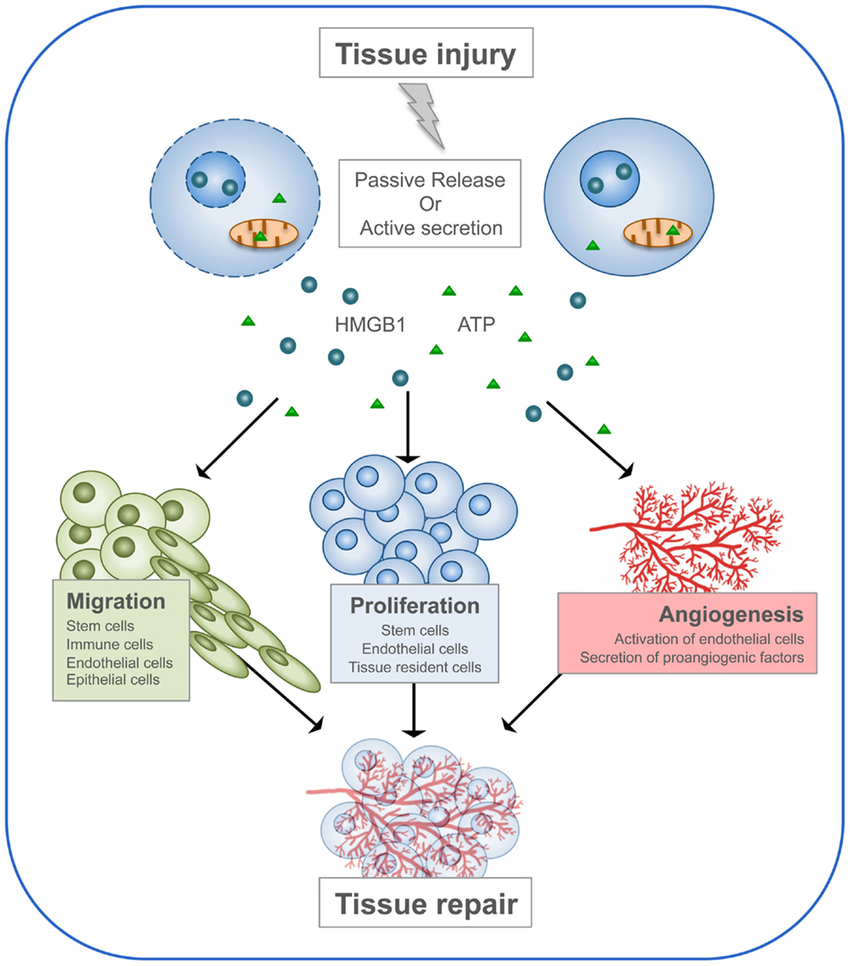
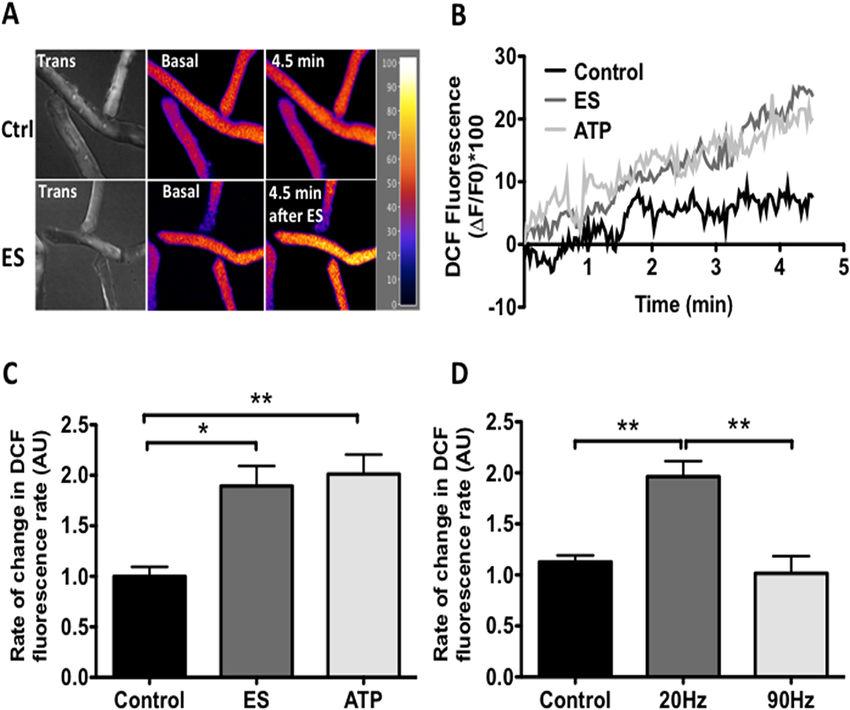
Cellular Electrostimulation: CellStim Microcurrent Therapy (CMT) involves the application of low-level electrical currents in microamperes through an advanced waveform encompassing a fast rise-time and an exponential fall-time. Monophasic anodal and biphasic pulses refer to a unidirectional or alternating flow of current, where the positive electrode (anode red connector) is applied on the sole of the affected foot. This electrical stimulation influences cellular activities, including the migration and proliferation of cells involved in the healing process.
ATP Production: CMT enhances adenosine triphosphate (ATP) production. ATP is an essential molecule that stores and transports energy within cells. Increased ATP levels accelerates cellular metabolism and improves the energy status of cells involved in tissue repair.
Cellular Migration: The electrical currents facilitate the movement of cells involved in tissue healing, such as fibroblasts and macrophages, to the site of injury. Improved cellular migration enhances the overall healing process by recruiting necessary cells in the affected tissue area.
Anti-inflammatory Effects: CMT with biphasic and monophasic anodal pulses have been studied and found to initiate anti-inflammatory effects, thereby reducing inflammation associated with plantar fasciitis. Controlling inflammation is essential for initiation of tissue healing, as chronic inflammation impedes normal tissue healing.
More info can be found here: www.cellstim.net/conditions/inflammation

CellStim Therapy Parameters
Frequency: 0.3 Hz
Intensity: 300 uA or sub-threshold
Polarity: Positive + and Monophasic
Duration: one hour per day
Pad Placement
Place red connector pad over metatarsophalangeal joints of the affected foot and white wire lead pad at inner ankle point K3.
Alternate K3 white connector pad to heel of foot.


References
The Effect of Monophasic Pulsed Current with Stretching Exercise on the Heel Pain and Plantar Fascia Thickness in Plantar Fasciitis: A Randomized Controlled Trial (Mar 2020)
https://www.mdpi.com/2227-9032/8/2/79
Applying 12-session of MPC results in significant reduction of heel pain and sagittal thickness of plantar fascia and that this treatment can be applied in the clinical setting since many of the electrical stimulation units include the MPC mode that we used in our study. Negatively charged cathode was used to attract the positively charged fibroblast cells to promote and accelerate proliferation phase of plantar fascia in the present study which may help decrease plantar fascia thickness.
Use of low-frequency electrical stimulation for the treatment of plantar fasciitis (Nov 2009)
https://pubmed.ncbi.nlm.nih.gov/19917733/
Results: Participants in the control and experimental groups demonstrated pain reduction and improvements in functional activity levels after 4 weeks and 3 months.
The Effect of Microcurrent-Inducing Shoes on Fatigue and Pain in Middle-Aged People with Plantar Fascitis
Intrinsic foot strengthening and electrostimulation in older adults – Randomized clinical trial (Feb 2023)
https://www.scielo.br/j/fm/a/3FHVYGnd4GsJngTYkqMm8ZL/?format=pdf&lang=en
Conclusion: An exercise protocol associated with electrostimulation improves performance in func-
tional and dynamic balance tests in older adults.
Electrical Stimuli Release ATP to Increase GLUT4 Translocation and Glucose Uptake via PI3Kγ-Akt-AS160 in Skeletal Muscle Cells (May 2013)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3636621/
Pulsed Electrical Stimulation Affects Osteoblast Adhesion and Calcium Ion Signaling (Aug 2022)
https://www.mdpi.com/2073-4409/11/17/2650
Chiropractic treatable conditions:
Correlation between COVID-19 vaccination and inflammatory musculoskeletal disorders (Nov 2023)
https://www.medrxiv.org/content/10.1101/2023.11.14.23298544v1
At 12 weeks after vaccination, the incidences of plantar fasciitis (0.14-0.17%), rotator cuff syndrome (0.29-0.42%), adhesive capsulitis (0.29-0.47%), HIVD (0.18-0.23%), spondylosis (0.14-0.23%), bursitis (0.02-0.03%), Achilles tendinitis (0.0-0.05%), and de-Quervain tenosynovitis (0.04-0.05%) were higher in all three vaccinated groups (mRNA, cDNA, and mixing and matching vaccines) when compared to the unvaccinated group. All COVID-19 vaccines were identified as significant risk factors for each inflammatory musculoskeletal disorder (odds ratio, 1.404-3.730), except for mixing and matching vaccines for de-Quervain tenosynovitis.
